
Nat’s story – “Being a young carer can be lonely”
Nat reflects on her experience of being a young carer and the support she received from the Nationwide dementia clinic.
Dementia is a progressive condition, and currently, there is no known cure. However, for some types of dementia, medication may help to relieve some of the symptoms or slow its progression. Our dementia specialist Admiral Nurses explain some of the medication options and how to support a person with dementia to take their medicines.
Medication for dementia is mostly prescribed for Alzheimer’s disease. However, people with other forms of dementia may also benefit from taking medication.
The main types of medication for Alzheimer’s disease are called ‘cholinesterase inhibitors’. They do not cure dementia or stop it worsening, but may slow down the progression and ease some of the symptoms.
There are three types of cholinesterase inhibitor that may be used for Alzheimer’s disease:
Cholinesterase inhibitors are usually prescribed for people with early to middle stage dementia, and tend to be most effective in the first six to 12 months of taking the medication.
Some people may be prescribed another medication for Alzheimer’s disease, called memantine. It is most often used for people who cannot take cholinesterase inhibitors, usually due to side effects or other medical conditions. It may be taken alongside a cholinesterase inhibitor in the middle to later stages of dementia.
Medications for Alzheimer’s disease do not help with vascular dementia. However, people living with vascular dementia – which is caused by problems with blood supply to the brain, for example as the result of a stroke or transient ischaemic attack (TIA, or ‘mini stroke’) – may be prescribed medicines to help with the underlying causes. These include medication for high blood pressure, high cholesterol and heart disease.
Some people with Lewy body dementia may be prescribed a cholinesterase inhibitor or memantine. They may also be prescribed antipsychotic medication to help with hallucinations, but this should only be used in severe cases as they can cause significant side effects.
People with frontotemporal dementia are generally not prescribed Alzheimer’s medication as it could make the symptoms worse. However, some people with frontotemporal dementia might be prescribed a specific type of antidepressant called a ‘selective serotonin reuptake inhibitor’ (SSRI) to help with uninhibited or compulsive behaviour and overeating.
There is no specific medication for mixed dementia – where two or more forms of the condition occur together – but if the person’s dementia is thought to include Alzheimer’s disease, they may be prescribed a cholinesterase inhibitor.
Dementia is common in people with Huntington’s disease. There is no specific medication to treat this condition, but people with the diagnosis may be prescribed medicines to help with specific symptoms such as depression and twitching/jerking movements.
Parkinson’s predominantly affects movement, but around one third of people with the diagnosis go on to develop dementia. While it cannot be cured, many people will take a drug called dopamine to help manage the symptoms. People with Parkinson’s dementia may also be prescribed a cholinesterase inhibitor.
PCA is a rare type of dementia that most commonly develops between the ages of 50 and 65. Cholinesterase inhibitors may be helpful for people with PCA.
Young onset dementia refers to any form of dementia that develops before the age of 65. There is no specific medication for young onset dementia, but a person with the condition may be prescribed the medication suited to their particular form of dementia.
Dementia medications work in different ways. For example:
Before starting medication for dementia, it is important to weigh up the pros and cons in conjunction with the doctor. They will carefully consider:
All medications have some risk of side effects. These are listed in the patient information leaflet which comes in the packaging.
Common side effects of cholinesterase inhibitors include:
Common side effects of memantine include:
Some side effects may only occur when first starting the drug or when increasing the dose. To minimise the risk, the prescriber will often start with a low dose of medication and gradually increase it.
If you need advice around side effects, you can speak to the person’s doctor or a community pharmacist.
When someone takes more than one medication they may interact with each other, causing side effects or reducing their effectiveness. Drugs for dementia may interact with other medications, for example antipsychotics or tricyclic antidepressants, so the doctor will always consider what medicines the person already takes before deciding whether to prescribe dementia medication.
A person with dementia may need support with managing their medication – for example remembering to take it, taking the correct dose at the right time and storing it safely.
Thanks for downloading! We’re only asking for your email so we can measure downloads and ask for your feedback. We won’t sign you up for any marketing communications, but if you'd like to stay in touch, sign up for our newsletter by clicking "Subscribe to our newsletter" at the bottom of this page.
The person with dementia should have regular medication reviews with their GP, community pharmacist or memory clinic.
If their medication is working, their symptoms will usually improve for around six to 12 months, but then they will gradually get worse. However, the person may continue to take the medication to avoid a sudden worsening of symptoms.
Dementia medicines do not work for everyone. Some people need to try several types to see which works best, and some find there is no benefit at all.
People may stop taking dementia medicines for a variety of reasons, including:
Stopping medication may be a personal choice or advised by the person’s healthcare professional. Ideally, it should be a joint decision.
If someone wishes to stop taking their medication, they should speak to their doctor first to ensure it is done in a safe and supervised way.
It is important for the person with dementia to take their medications as prescribed. To help the person remember to take their medication, you could try:
In some cases, pharmacies can supply tablets in a dosette box – a pre-filled pill organiser that clearly shows the times and days when each medication needs to be taken.
If a person with dementia forgets a dose of their medicine, they should take it as soon as they remember. However, if it is within four to six hours of their next dose, they should skip the missed dose completely.
Missing the occasional dose is unlikely to cause problems, but if this becomes a recurring issue, speak to the person’s GP or prescriber about why this is happening and whether it is still appropriate for them to take the medication.
If you need advice on any aspect of dementia, please call the Dementia Helpline on 0800 888 6678 (Monday-Friday 9am-9pm, Saturday and Sunday 9am-5pm, every day except 25th December), email helpline@dementiauk.org or you can also book a phone or virtual appointment with an Admiral Nurse.

Nat reflects on her experience of being a young carer and the support she received from the Nationwide dementia clinic.
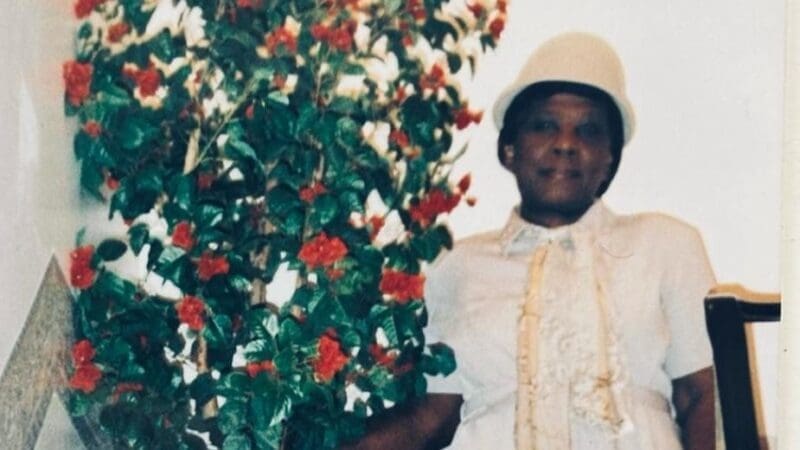
Tim reflects on the stigma that is often attached to dementia and the importance of the Black, African and Caribbean Admiral Nurse clinics.

Katrina reflects on the support she has received from her Admiral Nurse, Rachel, since her husband was diagnosed with young onset dementia.
A person with dementia might need support with taking their medication correctly. You can help them by:
Any decision about whether to take medication and if so, which one, will be carefully weighed up by the prescriber with the full involvement of the person with dementia and their family.
Stopping medication suddenly may cause a worsening of dementia symptoms, so it should always be done under medical supervision. Typically, stopping medication should be done slowly over the course of several weeks, watching out for any deterioration in the person’s condition.
However, many people will continue to take dementia medication until they are nearing the end of life, even if the benefits seem to be minimal.
Generally, alcohol should be avoided if a person is taking dementia medication because it can stop it working as well as it should and increase the risk of side effects. However, many people with dementia do continue to enjoy an alcoholic drink.
You can speak to the GP or pharmacy if you need advice about drinking alcohol while taking dementia medication.
This will depend on what type of phone you have. However, generally you can do this by going into the ‘Medications’ section of the Health app that comes preinstalled. There are also a number of medication reminder apps that you can download if you prefer.