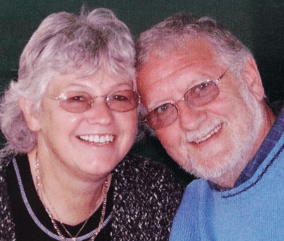
I still cherish every moment I have with Jan – Bob’s story
Bob, who has been married to Jan for 62 years, reflects on their beautiful relationship in spite of a heartbreaking journey with dementia.

How to support someone with a learning disability and dementia.
People with learning disabilities, including Down’s syndrome, are more likely to develop dementia. Our specialist Admiral Nurses, along with MacIntyre – the learning disability charity – share their expert advice.
In recent years, the number of people with learning disabilities being diagnosed with dementia has grown. This is partly because people with learning disabilities are more likely to develop dementia, and partly because life expectancy for people with learning disabilities is increasing all the time – and the risk of developing dementia increases with age.
People with a learning disability are also more likely to develop young onset dementia (where symptoms begin before the age of 65) – particularly people with Down’s syndrome.
Dementia in people with learning disabilities often progresses, or appears to progress, more rapidly if it is not diagnosed promptly.
Often, memory loss is one of the first signs of dementia, but people with a learning disability may show other symptoms first, such as:
If these changes are persistent, getting worse or affecting the person’s daily life, you should book an appointment with their GP. It is helpful to keep a record of their symptoms; if the person is under 65, you could use the Young Dementia Network’s personal checklist for this.
Anyone over the age of 14 who has a learning disability should have an annual health check with their GP to identify any health problems they are experiencing, including dementia. To ensure the person is offered this check, you can ask the GP to include them on the practice’s learning disability register.
The GP should start by assessing whether the person has an underlying condition that could cause similar symptoms to dementia, eg:
To rule out underlying conditions, the GP may suggest doing blood tests and a urine sample. If the person is unable or unwilling to consent to these tests, ask the GP about other ways to make an assessment.
The GP may briefly test the person’s cognitive abilities and short-term memory by asking them to name some common items, remember a name or address, and draw an everyday object, usually a clock. Some people struggle with these tests because of their learning disability rather than dementia; tell the doctor if this is likely to be the case.
If other conditions are ruled out, the GP may refer the person for further assessments. These are typically carried out at a memory clinic, but assessing a person with a learning disability can be more difficult and so should include a multidisciplinary team that includes a:
Do not be afraid to ask for reasonable adjustments to support the person – for example, allowing extra time to answer questions, ensuring the environment is calm and quiet to help them focus, and providing information in accessible formats, such as easy-read versions of written resources.
If the person is diagnosed with dementia, the health professional should tell you what type they are thought to have and what will happen next in terms of treatment options, referrals to other specialists, and support you can access.
Getting a diagnosis of dementia can be difficult for a person with learning disabilities. Understanding of learning disabilities and dementia amongst healthcare professionals is variable, and dementia symptoms are often put down to the person’s learning disability. In some cases, specialist dementia services like memory clinics do not even accept referrals for people with learning disabilities.
If you need support with getting a diagnosis of dementia for a person with learning disabilities, please call our free Helpline on 0800 888 6678 to speak to a specialist dementia nurse.
Living with a learning disability and dementia can be challenging for the person, their family and other people who support them. However, the right care and support can help everyone manage these challenges as well as possible.
In addition to seeing their usual health and social care team, the person may be referred to other professionals like a social worker, occupational therapist or psychiatrist. Where possible, keep the person informed about any changes to their care team.
To establish what support the person needs, including home adaptations, assistive living equipment and paid care, and any available funding for these, you can request a needs assessment through Social Services.
Families and carers who support the person could also consider enrolling in carer education programmes that are available from organisations like Dementia Carers Count and tide.
Support groups can be a great source of support and companionship for the person with learning disabilities and their carers. You can ask your GP, social worker or council for information on local services, such as MacIntyre Memory Cafés for people with learning disabilities and dementia.
As far as possible, help the person keep to their usual routine and continue with activities they enjoy, with adaptations and support if necessary – making big or sudden changes can be confusing and distressing. Give them more time for daily tasks and help them maintain as much independence as possible, with support if needed.
Whether the person with a learning disability and dementia lives independently, with family or in supported accommodation, take a look at their home environment to identify ways to keep them safe and help them maintain their independence. For example:
If the person lives in supported accommodation or a group setting, staff and other residents will need to be aware of their dementia diagnosis and how it affects them. Easy-to-read leaflets are available from MacIntyre.
If the person lives with family, it is important to consider how their care may need to be adapted as their dementia progresses. For example, if they live with elderly parents who are frail or have health and/or mobility conditions, a paid home carer could relieve some of the strain.
If the person eventually needs additional support from a home carer or to move into a care home, staff will need specialist knowledge and skills to support their needs. Some care homes will accept people with mild to moderate learning disabilities, but a specialist home may be more suitable for a person with complex needs. Again, include the person in these decisions as far as possible.
People with learning disabilities and dementia may have difficulties communicating, understanding, and/or processing and remembering information, so be prepared to change how you communicate. For example:
It is a good idea to help the person create a life story – a record of important information such as their personal details, past and current life and future hopes. This can help other people, including carers, better understand and communicate with them.
To ensure the person with dementia and a learning disability is well supported in the future, it is important to make:
An advance care plan: this sets out the person’s wishes for their future care, such as where they would like to be cared for and medical treatments they do/do not want. This is not legally binding but will help guide their care. You should work with the person’s care team to create this plan, involving the person themselves as fully as possible. We have a template you can use.
Lasting power of attorney (LPA): this is a legal document that enables you and/or other named people to make decisions about the person’s health and welfare and/or property and financial affairs if they lack the mental capacity to do so themselves.
If the person with learning disabilities does not have an LPA, they should make one as soon as possible. If they do not have the capacity to make an LPA, a health or care professional may need to work with you, the person and other carers to make decisions on their behalf, in their best interests.
The equivalent of an LPA in Scotland is called power of attorney; and in Northern Ireland, enduring power of attorney.
To speak to a dementia specialist Admiral Nurse about learning disabilities and dementia please contact our free Helpline on 0800 888 6678 (Monday-Friday 9am-9pm, Saturday, Sunday and bank holidays 9am-5pm, every day except 25th December). Alternatively, you can book a phone or video appointment.
macintyrecharity.org
General enquiries: 01908 230100
Email: hello@macintyrecharity.org
Our virtual clinics give you the chance to discuss any questions or concerns with a dementia specialist Admiral Nurse by phone or video call, at a time that suits you.
Bob, who has been married to Jan for 62 years, reflects on their beautiful relationship in spite of a heartbreaking journey with dementia.

Julie Hayden was diagnosed with dementia at just 54 years old. She's since dedicated herself to advocating for people living with dementia and elevating the voice of lived experience.
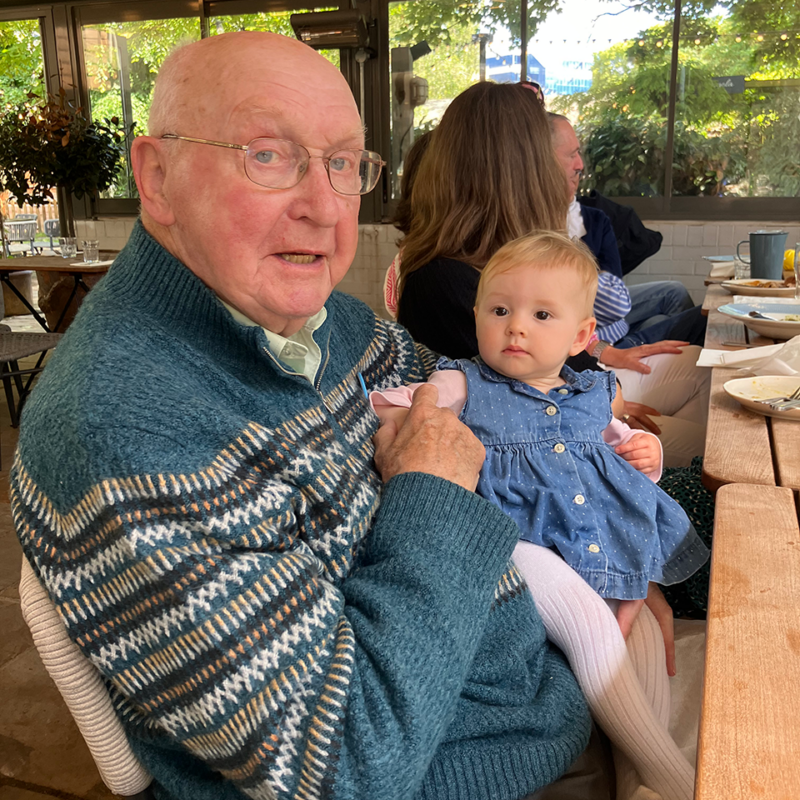
Simon, who has lived in New Zealand for two decades, discusses how he cares for his dad who has Alzheimer’s disease and lives alone in the UK.