
Specialist dementia support for the LGBTQ+ community
Our newly created Consultant Admiral Nurse service for the LGBTQ+ community is an exciting step for Dementia UK.
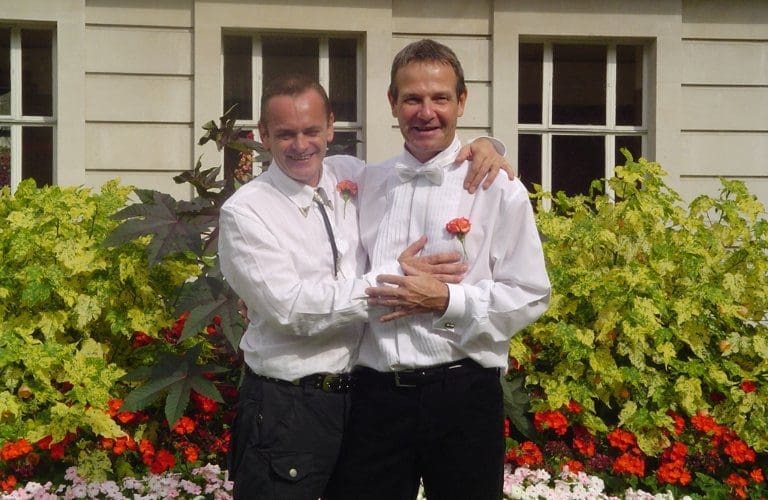
Mike and Tom’s story shares the impact dementia had on their marriage, and some of the unique challenges they faced as an LGBTQ+ couple.

Mike and Tom
So many people look back on their younger years with fondness. I envy that.
I look back on days filled with heartache and shame, guilt, and most importantly, fear. Like so many people in the LGBTQ+ community, I had to hide my sexuality for a very long time.
In the early 1970s, I saw a sticker one day on the London Underground advertising a social group for young gay people. I kept going up and down the escalator trying to discreetly write the number down – we didn’t have mobile phones in those days! After some time, I plucked up the courage to call and agreed to attend a tea party the next weekend.
Full of nerves, I walked in and sat down. A handsome man was sitting at the opposite end of the sofa. His name was Tom. He smiled at me and we started chatting. It’s fair to say I fell for him straight away.
That was the beginning of a 47-year partnership.
Loving Tom meant the world to me. And yet, I still felt the need to hide his existence from other parts of my life.
I worked in the London Fire Brigade for many years, and not once did I let on that I was gay, let alone that I had a partner.
In public, we didn’t hold hands.
The truth is, we were scared. Yes, times were changing for the better, but when you’re conditioned that any sign of gay intimacy comes with the threat of abuse or violence, it’s a very hard thing to unwind.
In 2008, Tom was diagnosed with mild cognitive impairment. But this later changed to a rare form of dementia, cortical basal degeneration.
I retired from my job in the Fire Brigade in 2014 to care for Tom as by this time, his cognitive and physical had issues became more complex. We’d go out for a walk, or a coffee, and he would be unsteady on his feet, so I held his hand. I did it so that he didn’t fall – but for the first time in my life, I did it without fear. I honestly didn’t care what people might have thought. A few times, passers-by did say nasty things – and I confronted them. I told them that this was my husband Tom, and that he had dementia.
When we attended appointments, health professionals would always assume I was Tom’s carer or another relative, never his husband. I wish they had just asked, “How are you connected to Tom?”
Assumptions like this are hurtful and disrespectful and can lead to poorer health management. They’re also one of the reasons people from the LGBTQ+ community are less likely to seek support. Even if stigma isn’t present, the fear of stigma can be just as powerful. I know this all too well.
We have come a long way in recent years and the increase in awareness-raising and training has been monumental. The most important thing is that the person on the receiving end of care feels supported and understood.
I am blessed to have cared for Tom at our home until he passed away in September 2022. Caring for him taught me how to let go of fear. It inspired me to help others in the LGBTQ+ community to feel safe and to expect respectful and relevant health support.
This starts with visibility. When Tom received his dementia diagnosis, we were invited to a support group of about 30 people, and we were the only gay couple. It took a lot of courage to say, “This is my husband.”
Everyone was accepting, but what was missing was other people from the LGBTQ+ community who might have had a shared lived experience and history. I couldn’t find any existing services, so I created one – what eventually became the LGBTQ+ Dementia Advisory Group. It was something that I needed as a carer to manage the stress and exhaustion of caring along with support through anticipatory grief and learning from others’ experiences.
The group has regular networking opportunities for people affected by dementia who identify as LGBTQ+. We also share knowledge, best practice and useful resources. We deliver training, web-based seminars and input and advice to many platforms discussing dementia, including health and care providers. We also contribute to academic projects aimed at addressing diversity and inclusion of LGBTQ+ people with dementia and their careers in services.
Having a dementia diagnosis and being from the LGBTQ+ community is complex and challenging, especially where services are broadly heteronormative. But in the group, you don’t have to explain the LGBTQ+ context so you can focus on the real experiences of living with dementia and push for meaningful change now and in the future.
We want people from this community to know that they are safe and accepted and look towards entering the world of care with the hope of respect, dignity, and relevant and safe care.
What a gift that is.
You can find out more about the LGBTQ+ Dementia Advisory Group here.

Our newly created Consultant Admiral Nurse service for the LGBTQ+ community is an exciting step for Dementia UK.

LGBTQ+ Dementia Advisory Group member Dáithí on the importance of using inclusive language and having a person-centred approach to care.
Doctors typically use the word ‘dementia’ to describe common symptoms – such as memory loss, confusion, and problems with speech and understanding – that get worse over time. Each type of dementia stops a person’s brain cells (neurones) working properly in specific areas, affecting their ability to remember, think and speak.