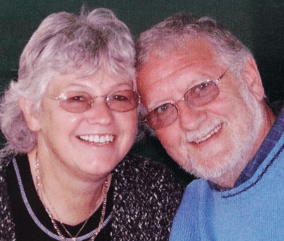
I still cherish every moment I have with Jan – Bob’s story
Bob, who has been married to Jan for 62 years, reflects on their beautiful relationship in spite of a heartbreaking journey with dementia.
Some people believe that people with dementia don’t feel pain, but this isn’t true. It can, however, be hard to tell if they are in pain, meaning that it is not treated properly. This can cause discomfort and distress.
The most obvious way to find out if a person with dementia is in pain is to ask them – but as their condition progresses, they may have difficulty telling you.
They may not be able to describe where the pain is coming from, and even say “no” if you ask if they’re in pain.
They might use the wrong words to explain how they feel – for example, saying “injection” rather than “indigestion”.
It may help to ask specific questions, such as:
Signs of pain to look out for include:
You could also try to think back to how they acted when they were in pain prior to their diagnosis, as you may be able to spot similar signs in their behaviour.
Investigating why the person with dementia is in pain will not only help them be more comfortable but also avoid medication being prescribed unnecessarily for symptoms like restlessness or agitation that could be relieved by treating their pain.
Possible causes of pain include:
Health conditions
People with dementia, especially those who are older, often have other health conditions as well. It is important to keep up with regular health checks and help the person take any prescribed medication correctly to try to keep them as well as possible.
Mouth problems
Gum disease and other mouth problems can be extremely painful. People with dementia may find it hard to maintain good oral health, but with support, they can brush their teeth daily, use a mouthwash and visit the dentist regularly. Read our information on mouth care for more advice.
Arthritis
Arthritis becomes more common as people get older, and can cause pain in the hands and feet, limbs, neck, spine, and sometimes torso. If you notice swelling, redness, or stiffness in the joints, speak to the person’s GP or a pharmacist for advice.
Constipation
Constipation can cause pain and discomfort, and is more likely if the person has a limited diet and/or is becoming less mobile.
Try to encourage them to eat a balanced diet with plenty of fresh fruit and vegetables, and ensure they are drinking enough fluid – our information on eating and drinking may be useful. If constipation is occurring frequently, speak to their GP or a pharmacist.
Inactivity
Lack of movement can contribute to pain, so if the person spends long periods in bed or a chair, encourage them to get up regularly if possible and support them to take a walk into the kitchen for a drink, or just around the room.
Being poorly positioned can also cause pain, so check that the person’s chair is supportive, and use cushions to help them sit comfortably. You can request a free Needs Assessment to identify any equipment or home adaptations that may improve their comfort and mobility.
The following strategies may also help relieve pain in a person with dementia.
Heat or cold can help with localised pain. Heat (such as a hot water bottle in a cover) is best for easing aches and stiffness. Cold (such as an ice pack) is better for treating inflammation like sprains and bruises.
Physiotherapy or massage can be good for soreness, stiffness and general aches and pains, but it’s important to explain what is going to happen and stop if the person seems to be in distress or discomfort.
Relaxation techniques such as breathing exercises or mindfulness can help.
Many causes of pain can be eased using the tips above, but sometimes, painkillers may be helpful, so consider making an appointment with the person’s GP.
It can be useful to keep a diary, recording things like:
If medication is recommended, support the person to take it as prescribed, and to attend any reviews with their GP or a nurse.
If the person has difficulty taking tablets, speak to the GP about other options, such as patches.
If you have any questions or concerns relating to dementia, call our free Dementia Helpline on 0800 888 6678 (Monday-Friday 9am-9pm, Saturday and Sunday 9am-5pm), email helpline@dementiauk.org or you can book a virtual appointment with an Admiral Nurse via phone or video call.
You may also find the following information useful:
Our free, confidential Dementia Helpline is staffed by our dementia specialist Admiral Nurses who provide information, advice and support with any aspect of dementia.
Bob, who has been married to Jan for 62 years, reflects on their beautiful relationship in spite of a heartbreaking journey with dementia.

Julie Hayden was diagnosed with dementia at just 54 years old. She's since dedicated herself to advocating for people living with dementia and elevating the voice of lived experience.
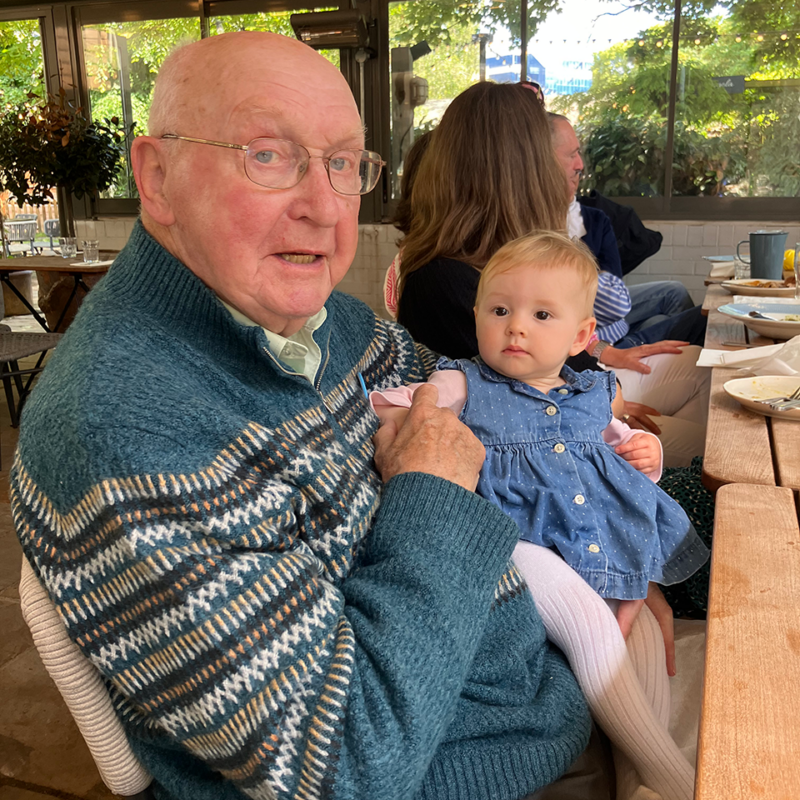
Simon, who has lived in New Zealand for two decades, discusses how he cares for his dad who has Alzheimer’s disease and lives alone in the UK.