
Sarah’s story – “Dementia UK was our saving grace”
Sarah reflects on reaching crisis point when her husband, David, was diagnosed with young onset dementia and the support her family have since received from Dementia UK.
Caring for a person with dementia affects the whole family and bring new challenges every day. Carers often tell us that they struggle to find support and are sometimes left feeling exhausted, overwhelmed and alone. But many also share moments of joy and closeness with the person they care for, and make new memories together.
Understanding the changes in the person with dementia and making sure you receive the support you need to care for them can help you stay physically and mentally well, maintain your relationship with them and find time for yourself outside your caring role.
Family carers and our dementia specialist Admiral Nurses share their personal insight into what it’s like to care for someone living with dementia, and their tips for coping.
There are many types of dementia, each with its own symptoms. The most common forms are:
It’s important to note that everyone will have their own unique experience of dementia, with their own strengths and challenges. And as it progresses, people are likely to develop a wider range of symptoms, with more overlap between the different types.
Everyone’s journey with dementia is different. While it’s most commonly associated with memory loss, the symptoms are wide-ranging. Understanding how it affects the person you are caring can help you provide the right support and develop strategies to cope with the changes.
These are some of the symptoms you might see in a person with dementia.
Memory problems – particularly with short-term memory – are common in people with dementia, especially those with Alzheimer’s disease. The person might forget recent events, repeat themselves in conversations, forget names and places and misplace items or put them in the wrong place.
A person with dementia might struggle with concentration, attention, problem-solving and decision-making. They may show changes in behaviour, for example obsessive, compulsive or uninhibited behaviour. Communication difficulties are common. Many people also experience sundowning: a state of intense confusion and anxiety that typically occurs around dusk and often causes a strong sense of being in the wrong place.
“In recent years, Dad has been overcome with confusion once the sun goes down – known as ‘sundowning’. Despite the fact it’s pitch-black outside, he believes that it’s daytime, so it’s very hard to get him to sleep at night. As a result, I’ve had to adjust my own sleeping patterns, often staying awake for most of the night and napping throughout the day.”
– Kaur, who cares for her dad, Mohinder
People with dementia may experience changes in personality, which can be upsetting for their carers. They might lack empathy, lose motivation and interest in their daily activities and the people around them, or become uncharacteristically irritable and aggressive.
“Carol became aggressive, which was distressing for both me and our children. She would verbally abuse me, and it felt like whatever I did was wrong. But Admiral Nurse Katie really listened to me and reassured me that I wasn’t doing anything wrong, that Carol’s behaviour was just part of the disease.”
– Russell, who cares for his wife, Carol
People with dementia may experience depression, anxiety and difficulty managing their emotions. This may be caused by dementia itself, or the impact of its symptoms on their daily life and the plans they had for the future. It might cause them to withdraw from other people.
“Sometimes I would have to remind Gopala to take a shower, or to brush his teeth. This would lead him to become incredibly frustrated. He would get angry at me, which was so out of character for him. However, I knew deep down he was just angry at his condition and his inability to do things he’d previously done with ease.”
– Pratibha, who cared for her husband, Gopala
Dementia can affect the senses, including how a person perceives things visually and responds to sensations like sound, touch and smell. For example, a reflection in the mirror might appear to be a person or animal in the home, or loud noise may make the person feel overwhelmed and distressed.
In some forms of dementia hallucinations are common, where the person experiences something that is not really happening. They might hear voices, see things that aren’t there or feel physical sensations that are not real, for example feeling bugs crawling on their skin.
Some people with dementia experience delusions: false beliefs that feel completely real, for example believing someone is trying to steal from them or thinking their partner is being unfaithful.
Dementia can lead to physical changes. In some forms of dementia, these can occur in the early stages: for example, people with Lewy body dementia may experience slowed movement, difficulty walking, tremors and falls.
As dementia progresses, a person may develop more physical symptoms, such as:
Caring for someone with dementia can be very challenging. It can be hard to see the changes in someone you love, and many carers and family members experience grief for the person even while they are still alive. Relationships may also change – for example, the person’s partner may feel more like a carer, and parent-child relationships may reverse.
Guilt is a common emotion. Carers may feel guilty if they feel they are not doing enough, or if they are sometimes frustrated or resentful of their caring duties.
As a person’s dementia progresses, the impact on those around them is likely to increase. For example, their carer may have to reduce their hours at work or stop working completely because of their caring responsibilities. Or their caring duties may affect their physical and mental health.
It’s very important to look after yourself if you care for someone with dementia so you don’t reach the point of burnout. Our advice on looking after yourself as a carer has tips to help you take care of yourself.
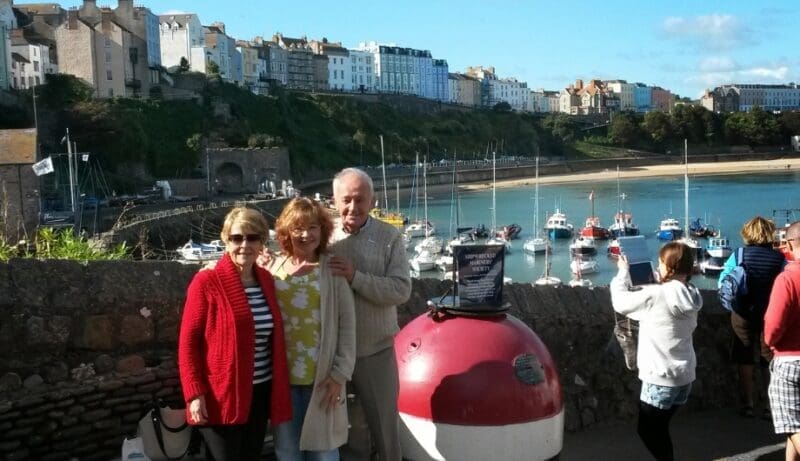
Bear in mind that while the caring role can be very difficult, you can still have a close and meaningful relationship with the person with dementia, even if it looks different from how it was before. For some people, a diagnosis of dementia can open up new opportunities – for example, to try a new hobby together, travel, or spend more time together as a family.
Even as dementia progresses, there can be moments of joy and connection that sustain you through the harder times. There may be opportunities to make new memories, even if the person with dementia can’t retain those memories themselves. Some carers also feel a sense of pride and fulfilment from being able to care for their loved one.
“I didn’t hesitate to fill the role of Nan’s primary carer. All of my life she had been there for me. Now it was my turn to be there for her. And even though the juggle of caring, full-time work and parenting was a lot, I never regretted this for a second.”
– Michaela, who cared for her grandmother
Caring for a person with young onset dementia (where symptoms develop before the age of 65) can be particularly difficult. You may face additional challenges such as juggling work and caring, looking after children or teenagers, and changes in your financial situation. Children may also find themselves in the role of young carer if a parent has young onset dementia.
Our Admiral Nurses are here to support you as the carer of someone with young onset dementia, and we also offer specialist support to children and young people. Please contact our Helpline if you need to talk to someone.
“Caring for a loved one with dementia is an emotional journey filled with moments of love, frustration, and intense guilt. I think it stems from love, because you want to do everything you possibly can. It doesn’t matter how much love, care and support you provide, you will always have feelings of not doing enough.”
– Ricky, whose gran had Alzheimer’s disease
“Mum will occasionally call me by her brother’s or my dad’s name, but we really get each other. She has good days and not so good days, but it’s impossible to be around her and not feel her passion for life.”
– Will, whose mum Ronnie has young onset dementia
“While Dawnie’s final years were incredibly hard to navigate, we were able to create memories that I never thought we would be able to. We took her on a helicopter flight. We did a birds of prey experience. Went on a holiday to Devon. Visited Cadbury World. And had many outings for coffee and cake – her favourite. This meant the world.”
– Rosie, who cared for her mum, Dawnie
“Living with dementia is hard. Your whole life changes. Relationship dynamics change. I’m Andy’s carer now – but I’m also still his partner. We go swimming in our local lake and have signed up for marathons. We have learnt we can live well with dementia if we make adjustments. It’s part of our life now.”
– Christine, whose partner Andy has young onset dementia
Dementia is a complex and challenging condition, whether you are living with it yourself or supporting someone with the diagnosis, but there are strategies to help you cope. Here are some tips.
Try to pre-empt the person’s needs: offer drinks, snacks or help with personal care at regular intervals to prevent distress.
You might be reluctant to tell people that you are a carer – perhaps because you feel you are simply doing what is expected in your relationship, or because you feel you should be able to manage without support. But it’s important that the people around you understand that you are caring for someone with dementia so they can offer support.
As dementia progresses, the person’s needs will increase and they will need more support. You can ask your local Social Services for a care needs assessment, which will help identify what support the person needs and any financial support that is available. You are also entitled to a carer’s assessment from Social Services which will look at what support you need in your caring role.
As a carer, accepting that a person needs additional support – whether from home carers or in a care home – can be difficult. It’s natural to feel like you should be able to cope, or that you’re letting the person down. But the right support can often free up time that was taken up with caring tasks, so you and the person with dementia can enjoy quality time and connection together.
“Even though I have now found the right care home for Mum, the feelings of guilt don’t go away but I try to consider what I would say to someone else in the same situation as me. Seeing that Mum is content and settled in the care home helps hugely and gives me some peace.”
– Penny, whose mum lives with dementia
If you are caring for someone with dementia, it’s essential to have support. This could come from:
Our Admiral Nurses are also here to answer any questions about dementia and offer practical advice and emotional support – you can contact our Helpline or book a video or phone appointment.

Sarah reflects on reaching crisis point when her husband, David, was diagnosed with young onset dementia and the support her family have since received from Dementia UK.
Claire's story shares the loss of both her parents, how Admiral Nurse Simon helped her and why she has donated to Dementia UK.

When Michaela’s grandmother, Vanda, was diagnosed with vascular dementia, she dedicated herself to creating a place where dementia wasn’t a taboo subject.
There will often come a point when a move to a care home is the best way to ensure the person’s safety, comfort and quality of life. This will depend on their individual circumstances, but signs it may be time to consider a care home include:
It’s natural to feel guilt, sadness or worry about moving a loved one into a care home. Our Admiral Nurses can help you work through making the decision, offering practical advice, emotional support and guidance on choosing the right care home.