Kerry’s story
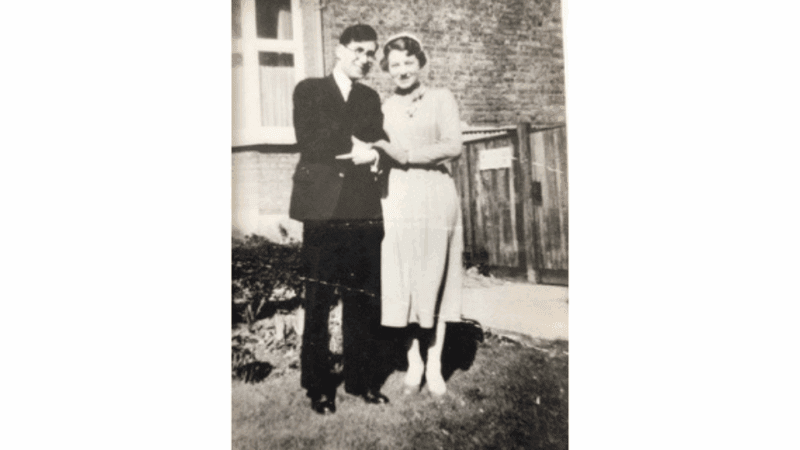
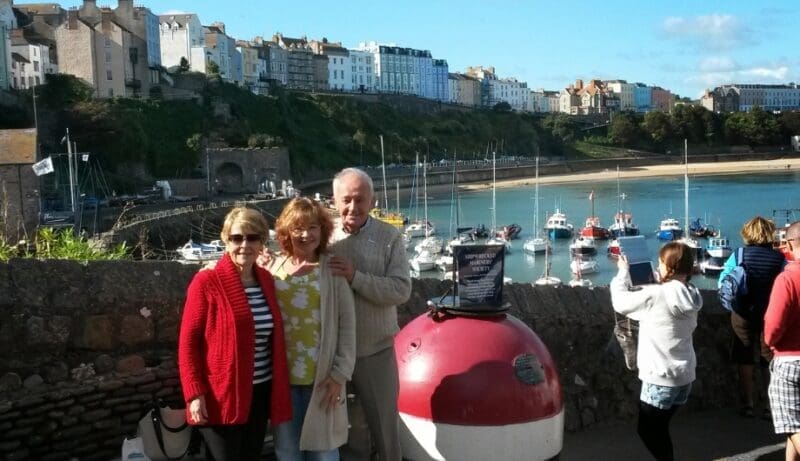
Kerry reflects on her mum's dementia journey and her experience doing two of Dementia UK’s virtual event challenges.
Delirium is a state of sudden, intense confusion. It is common in older people and those with dementia and can make them increasingly anxious and distressed. Our specialist Admiral Nurses explain the signs to be aware of and how you can help a person with dementia who is experiencing delirium.
Delirium is a state of intense mental confusion that comes on suddenly. It can have a big impact on the way a person behaves and functions, especially if they have dementia.
People with delirium typically become confused and/or disorientated and have difficulty concentrating. It can be very distressing for the person experiencing it and their carers.
There are three types of delirium: hyperactive, hypoactive and mixed. For older people, including those with dementia, hypoactive and mixed delirium are the most common.
Hyperactive delirium causes confusion that fluctuates throughout the day. A person who is experiencing hyperactive delirium may:
Hypoactive delirium is characterised by the person becoming less responsive. They may:
When someone is experiencing mixed delirium, they will have symptoms of both hyperactive and hypoactive delirium and may switch between them. A person with mixed delirium may be sleepy and unfocused one day, and agitated and restless the next.
It can be difficult to recognise delirium in people with dementia because many of the symptoms are similar: for example, confusion, memory loss and problems with concentration. However, it is important to know the signs and seek medical help quickly if you spot them.
The symptoms of delirium may be cognitive (affecting the person’s ability to remember, think and communicate), behavioural and/or physical. They include:
Older people with delirium and dementia often need longer stays in hospital, are more prone to falls or accidents, and are more likely to be moved into a care home.
Delirium is most common in older adults – particularly those over 80. There is also a strong link between delirium and dementia. Delirium is particularly common on hospital wards, affecting approximately 25-30% of older people and up to 50% of people with dementia. People living in care homes are also more prone to delirium.
There are a number of reasons why someone may develop delirium.
Medical conditions that can cause delirium include:
Environmental factors that can cause delirium include:
Some types of medication can make delirium more likely, especially if the person is taking multiple medications.
Up to 50% of older people who have surgery develop delirium. People who have hip surgery are at a particularly high risk, with research suggesting that 70-80% develop delirium.
Delirium is more common in people over 65; however, younger people can also be affected.
If a person is experiencing symptoms of delirium, it is important to seek medical advice. It can often be diagnosed based on their symptoms. Their healthcare professional should consider their:
The doctor may request blood and urine tests to check for underlying causes, such as an infection, constipation or difficulty passing urine. They should also review any medication that could be contributing to the delirium.
Treating delirium usually involves addressing any underlying causes. For example, if the person has an infection, they may be prescribed antibiotics, or if they are constipated, they may be given laxatives.
Medication is not usually given for delirium itself. If the person is particularly distressed, they may be given a short, low-dose course of medication such as a sedative or antipsychotic. However, for some people, particularly those with Lewy body dementia, these medications can make delirium worse, so they should only be used if absolutely necessary – for instance, if the person is at risk of harming themselves or someone else.
Sometimes, there is no treatable cause of delirium; in these cases, the person may just need support, time and rest to recover, ideally in a calm and familiar environment. Family members can help by reassuring them that they are safe, making sure that they are wearing their glasses or hearing aids, and encouraging them to eat and drink.
Delirium can be serious, so it is vital that the person receives medical assistance as soon as possible if you notice the symptoms. If the person is at home, contact their GP and ask for an urgent appointment. If they are in hospital, tell the nurse or doctor who is looking after them. If they are in a care home, tell a carer.
If you think the person is seriously or suddenly unwell, take them to A&E or call 999 for an ambulance: in rare cases, delirium or its underlying causes can be life-threatening.
You could also try these ideas to try to ease the person’s distress:
About 60% of people with delirium recover within a week. Some people, however, take longer to recover, and some never return to exactly how they were before – this is more likely if the person is living with dementia. You should also consider whether the person may be in pain (especially chronic pain such as arthritis), which has worsened, and they are struggling to communicate.
Delirium cannot always be prevented, but there are things you can do to reduce the risk.
When someone has delirium, the symptoms come on very quickly, over the course of one or two days or even a few hours, whereas dementia develops gradually over months or years. The symptoms of delirium also tend to vary a lot throughout the day.
Kerry reflects on her mum's dementia journey and her experience doing two of Dementia UK’s virtual event challenges.

Safia, a dementia specialist Admiral Nurse for the Black, African and Caribbean Communities, speaks to Elene, whose mum lived with dementia. They reflect on the importance of culturally appropriate dementia care and support.
Claire's story shares the loss of both her parents, how Admiral Nurse Simon helped her and why she has donated to Dementia UK.
To speak to a specialist dementia Admiral Nurse about alcohol-related brain damage or any other aspect of dementia, please call our free Dementia Helpline on 0800 888 6678 (Monday-Friday 9am-9pm, Saturday and Sunday 9am-5pm, every day except 25th December or email helpline@dementiauk.org.
If you prefer, you can book a phone or video appointment with a specialist dementia Admiral Nurse in our virtual clinics.
Sundowning is a state of intense confusion that occurs in many people with dementia, typically in the evening. A person who is experiencing sundowning will often be very anxious and confused, with a strong sense of being in the wrong place. Although the symptoms can be similar, sundowning is not a type of delirium. Read more about sundowning.
Most people with delirium start to improve within a few days, especially if the root cause is identified and addressed. Some people, however, take longer to recover and may have symptoms of delirium for weeks or months after initially becoming unwell. Some people never fully return to how they were before.
There is no specific cure for delirium. However, it can often be successfully treated if any underlying causes are addressed, for example by prescribing medication to treat an infection, and the person is well supported.
Delirium can indicate an infection which, if not treated, could lead to medical complications such as sepsis, which can become life-threatening.
Sundowning is a term used for the changes in behaviour that occur in the evening, around dusk, and experience agitation or anxiety.

Read personal stories from people living with a diagnosis, their family members and friends - as well as our dementia specialist Admiral Nurses.

Whether you have a question that needs an immediate answer or need emotional support when life feels overwhelming, these are the ways our dementia specialist Admiral Nurses can support you.