
Specialist dementia support for the LGBTQ+ community
Our newly created Consultant Admiral Nurse service for the LGBTQ+ community is an exciting step for Dementia UK.
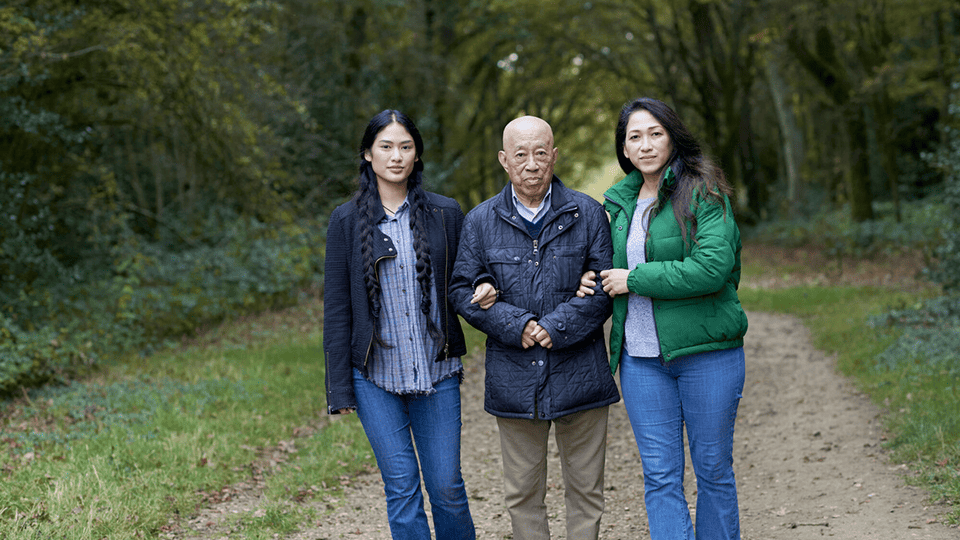
Admiral Nurse Asma Pandor discusses the importance of cultural and religious awareness within dementia care for ethnic minorities
There are an estimated 25,000 people in ethnic minority communities with dementia in the UK; there are varying experiences and care needs in each of these communities. While the number of white, British people with dementia is expected to double by 2051, the numbers of people from ethnic minorities is expected to increase seven-fold by the same time (Alzheimer’s society, 2019).
Although prevalence of dementia is higher in some ethnic minorities, they are also less likely to engage with dementia services. Research has suggested that until barriers such as stigma, communication problems and discrimination are explored and resolved ethnic minorities will continue to miss out on vital support.
Healthcare professionals require religious and culturally sensitive training and support in delivering person-centred care, or care which respects the needs, rights, wishes and experiences of every person. This is especially the case for those from ethnic minority communities who continue to under-access care because of a lack of tailored services.

As symptoms of dementia develop, there can be a tendency for long term memories to override short term memories; for people from ethnic minorities this can take them back to a time when they were conversing solely in their mother tongue, memories of their place of birth and other cultural experiences.
There is a lot of research which highlights the importance of considering the ‘super diversity’ of ethnic minority communities. The ability to acknowledge and respond to these specific cultural differences within ethnic groups is essential to ensure a holistic person-centred approach is met.
Interestingly, it has been suggested that standard tests for detecting dementia may not be culturally appropriate, consequently leading to flaws in diagnosis. Alzheimer’s Research UK state that the memory tests currently conducted compare performance to the majority white British population norms. The lack of culturally tailored questions on these tests could prove to be a huge hindrance in trying to reach a diagnosis of dementia in these communities.
All health and social assessments should take into account cultural factors. When determining a person’s needs and how they can be met, health and social workers should consider attitudes towards health, sickness and care, as well as the person’s family, personal history and religious beliefs. Considerations of any communication and language issues are important too.
All health and social care practitioners should work in a culturally competent way. This means being more aware of one’s own identity and how one may be perceived, but also approaching with an open mind, kindness and respect for all cultures and ethnicities. Culturally competent care and practice is more than just having the knowledge base around differing cultures; it is the ability to meet social and cultural needs of the individual regardless of their life and cultural experiences. Cultural competence is something that is absolutely vital when it comes to effectively delivering high-quality care, and without it, there will inevitably be poorer patient outcomes and a lack of patient satisfaction.
An elderly Indian Muslim gentleman with vascular dementia was admitted to Gloucestershire Royal Hospital where I am an Admiral Nurse. He required assistance with all activities of daily living (ADLs) including eating and drinking. There was also a language barrier as English was not his first language. As the individual was being assisted with his meal, a family member entered and noticed pork on the plate and asked for the meal to be discarded. The family member was devastated by this incident and asked for an explanation. Sadly, the staff were unaware of the religious beliefs of the person with dementia and thus unaware to any dietary requirements.
Upon hearing about this incident, I held a meeting with the family to apologise and assured them this would not happen again. The family were also encouraged to bring food from home which he would enjoy. I felt it was crucial to provide training sessions to help build awareness of different cultures and religions. Staff were reminded of the importance of finding out individual dietary requirements and ensuring this was clearly documented and handed over so all staff were aware.

Our newly created Consultant Admiral Nurse service for the LGBTQ+ community is an exciting step for Dementia UK.

Hannah Gardner has recently been appointed as Consultant Admiral Nurse for Children and Young People.
Admiral Nurse Lizzie Harrison provides support strategies for young people caring for someone with dementia.