
Cici and Izzy’s story – “I hope sharing our experience helps other young carers”
Cici (28) and Izzy (23) share their experiences of having a parent living with young onset dementia and becoming a carer at a young age.
Incontinence is when someone unintentionally passes urine (pee), known as urinary incontinence, or faeces (poo), known as faecal incontinence. Some people have both types, known as double incontinence.
Incontinence is common in people with dementia. This may be due to dementia itself, or other reasons such as physical health conditions and ageing.
Incontinence can be distressing for the person with dementia and those who care for them, and adds to carer stress. However, there are ways to manage incontinence and maintain the dignity of the person who is experiencing these problems.
Our dementia specialist Admiral Nurses explain why someone may develop incontinence, its effects and ways to manage the problem.
Signs of incontinence can include:
There may be less obvious signs of incontinence – for example, you may not realise the person has had an accident, but later discover they have hidden soiled clothing.
Incontinence may happen during the day and/or night (bedwetting).
The part of the brain that controls the bladder and bowels can be damaged in people with dementia, meaning they can’t tell when they need to empty their bladder or bowels.
Other reasons for incontinence in people with dementia include:
People are more likely to experience incontinence as they get older. It can also be linked to other health conditions, including:
Some medications have side effects that can cause or worsen incontinence, such as:
It is important that if you suspect any medications are causing incontinence, you monitor the situation and discuss any issues with the pharmacist or the doctor who prescribed them.
Continence can be a difficult or embarrassing topic to discuss, especially if the person hasn’t experienced it before. It is important to be patient and understanding. But speaking openly will encourage the person not to hide the problem, but to realise that it’s acceptable to talk about this issue, which will affect many people at some point.
Communicating honestly also means you can explore strategies together that will help you both cope better. For example, you could put reminders in the bathroom and place continence products in an easily accessible place, such as a small, discreet basket, rather than putting them away in a cupboard or another room.
If a person with dementia is experiencing incontinence, it is a good idea to book a check-up with their GP, as some causes can be treatable.
You can also arrange an assessment with an NHS continence service – you can ask the GP for a referral, or in some areas request the assessment yourself. These clinics are staffed by specialists who can investigate the causes of incontinence, suggest treatments that may help, and advise you on managing the problem.
District Nurses can also help with continence issues, so if you have contact with them, feel free to discuss your concerns and seek their advice.
While incontinence can be difficult for the person and those around them, it is possible to manage the condition and make it easier to cope with.
Understanding the person’s toileting habits can help you to create a routine with them and may reduce the number of accidents. This might include:
The person may feel embarrassed by conversations around needing the toilet. Instead, they may use euphemisms, such as “I need to go out,” so pay attention to what they’re saying and whether they might be trying to tell you they need the toilet.
The person may also hide wet or soiled clothing or bedding due to embarrassment. Instead of pointing this out, quietly remove the soiled items and replace them. Keep a linen basket in an obvious place and remind the person reassuringly what this is for.
Use appropriate continence products, as this can reduce some of the anxiety the person may feel about soiling their clothes.
Wet and soiled skin is more prone to sores and infections, so it’s important to help the person with dementia stay clean and dry. As soon as possible after an episode of incontinence, the person’s skin should be carefully cleaned with warm water and fragrance-free soap, or wipes that are specifically intended for this purpose.
It is particularly important to make sure the person’s skin is properly dry, especially in skin folds, to reduce the risk of fungal skin infections. The best way to do this is by patting dry rather than rubbing.
If possible, check for any sore or dry skin, as this may need treatment. If you have concerns about the person’s skin, book an appointment with the GP or Practice Nurse.
If you use barrier creams or ointments, be aware that they can reduce the absorbency of incontinence products.
There are many protective products for incontinence, including pads, disposable pants, bed and chair protection such as absorbent mats and waterproof sheets and adapted clothing.
Some of these may be available free of charge on the NHS. They are also readily available from pharmacies, some supermarkets and online.
The person’s district nurse or a continence clinic adviser can help you decide which products to use.
If you need to support a person with dementia to use the toilet, always offer as much privacy and dignity as possible. Smile and offer encouragement to prevent them feeling embarrassed and help them collaborate with you.
The person with dementia may need you to guide them to the toilet. You might need to help them with their clothes. If possible, encourage them to do it themselves in small steps: for instance, “Can you undo your zip? Now, can you pull down your trousers?”
Loose clothes such as tracksuit bottoms or clothes with Velcro fastenings might be easier for some people.
The person may need your help to sit down on the toilet. If they usually stand to urinate, encourage them to sit down at least once a day to open their bowels.
Allow the person plenty of time to use the toilet so they feel unhurried and relaxed. After use, you can check the toilet pan to see if they have passed urine or stools. If you notice any irregularities, such as blood, inform their GP or nurse promptly. Afterwards, encourage or help them to wipe themselves and wash their hands.
Eating and drinking can have an impact on how often someone needs to go to the toilet. To support them, it is important to:
This video provides tips on how to avoid it, what to do in the moment and how to get help.
To speak to a specialist Admiral Nurse about continence or any other aspect of dementia, please call our free Dementia Helpline on 0800 888 6678 (Monday-Friday 9am-9pm, Saturday and Sunday 9am-5pm, every day except 25th December), email helpline@dementiauk.org or you can book a phone or virtual appointment with an Admiral Nurse.
You may also find the following helpful:

Cici (28) and Izzy (23) share their experiences of having a parent living with young onset dementia and becoming a carer at a young age.

Nat reflects on her experience of being a young carer and the support she received from the Nationwide dementia clinic.
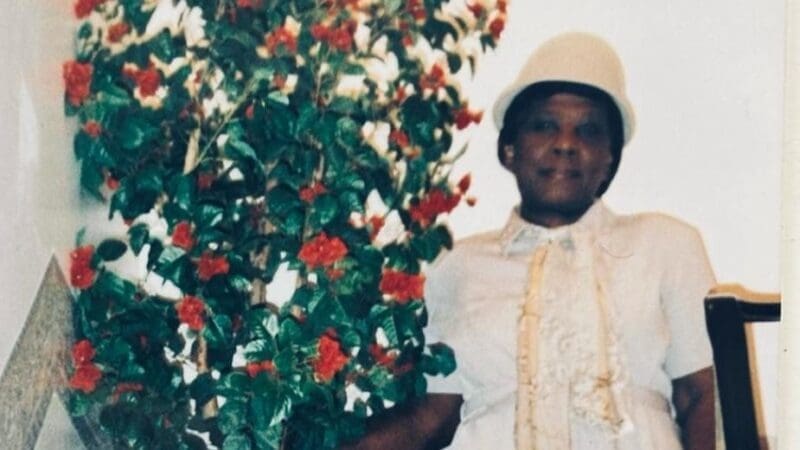
Tim reflects on the stigma that is often attached to dementia and the importance of the Black, African and Caribbean Admiral Nurse clinics.
Incontinence becomes more common as dementia progresses and is very likely in the late stages because of the deterioration in the person’s physical and cognitive abilities. However, it can develop in the earlier stages, for example in a form of vascular dementia called Binswanger’s disease.
Yes, incontinence is common in part of dementia. This is because of damage to the areas of the brain that affect bladder and bowel control, along with other physical and mental symptoms like mobility and communication problems.
Incontinence may not be preventable if it’s caused by damage to the parts of the brain that are responsible for our bladder and bowels. However, if it is caused by other symptoms of dementia, it may be manageable. For example, if communication difficulties mean the person can’t tell you they need the toilet, you may be able to work this out by watching their behaviour and non-verbal communication.