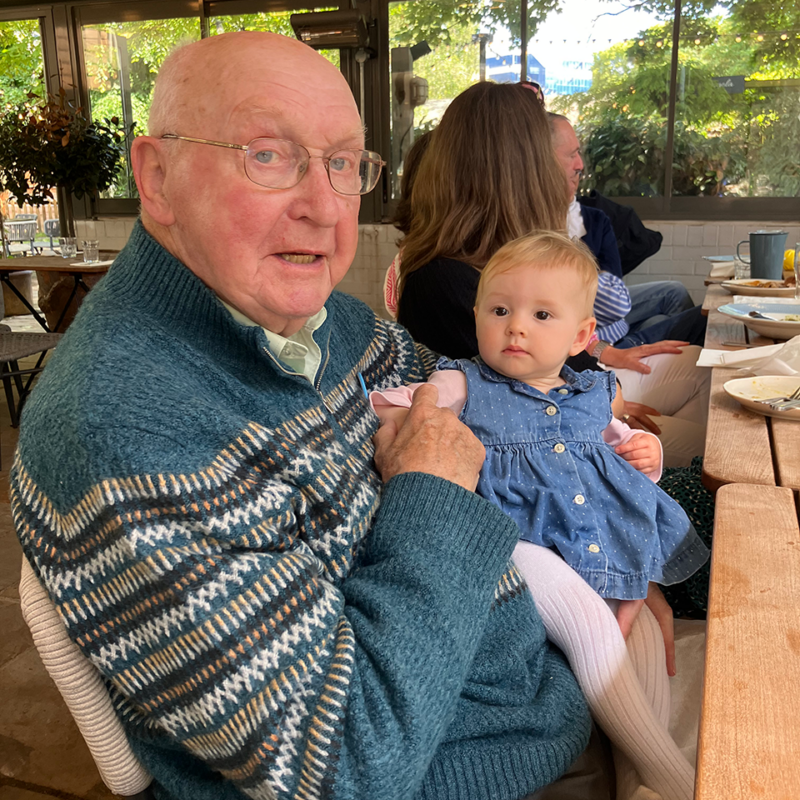
Caring for Dad, from near and afar – Simon’s story
Simon, who has lived in New Zealand for two decades, discusses how he cares for his dad who has Alzheimer’s disease and lives alone in the UK.
Caring for a person with dementia who also has cancer can be challenging. This guide will help you understand how it might affect the person you look after, and the treatments and support available.
Cancer is a disease which starts in cells in the body – the tiny building blocks that make up our organs and tissues.
Usually, cells divide in a controlled way – this is how our bodies grow, heal and repair.
But in cancer, a cell becomes abnormal and starts dividing uncontrollably, making more and more abnormal cells. These cells may gather to form a tumour.
Cancer cells can spread into the surrounding tissues and cause damage, and to other parts of the body through the bloodstream or lymph system to form secondary tumours.
A diagnosis of cancer can be extremely challenging for a person with dementia and their family. For example:
The main treatments for cancer are:
The cancer treatment offered to the person you are caring for will depend on factors like:
The person’s doctor (usually a specialist called an oncologist) will be able to discuss which treatments are most appropriate.
Some people with cancer and dementia will be able to have standard cancer treatment.
Others may have modified treatments that are less intense or invasive, such as a lower dose of chemotherapy or fewer treatments.
They will usually spend less time in hospital and have fewer side effects, but while these types of treatments may control the cancer, they won’t cure it.
If the cancer is advanced, the treatment doesn’t work, or it is decided that it would be inappropriate, the person can still be given treatment to help control symptoms such as pain.
This is called ‘supportive’ or ‘palliative’ treatment.
Before starting treatment, the person’s doctor will talk to them about what to expect, including:
After this, the person will be asked to sign a form saying that they consent to treatment.
However, for consent to be valid, the person must have ‘mental capacity’.
This is a legal term referring to whether the person is able to make important decisions.
To be considered as having capacity, the person must:
The doctor looking after the person with dementia may need to assess whether they have capacity.
If they don’t, a treatment or support plan will be drawn up in their best interests, considering any future care plans they made.
As the carer of someone with cancer and dementia, you may have to help them decide about treatment or make decisions for them, so it’s important to discuss how they would like to be cared for while they still have capacity.
This ensures that you, other family members and health and care professionals understand and respect their wishes.
With your support, the person may want to make:
The person with cancer and dementia is likely to have lots of medical appointments and hospital visits. You can support them by:
If possible, it’s important to help the person you care for to think ahead about where they will be cared for in the future.
Most people with long-term health conditions prefer to stay at home for as long as possible.
They may be helped by home carers and/or health professionals such as district nurses or palliative care nurses (nurses who provide support at the end of life).
Make sure you take into account your own ability to cope as a carer, and how you can access support.
If you and the person you care for wish for them to stay at home, short-term or respite care may be helpful for you both. This might be to have specialised care that helps control symptoms or to give you a break from caring.
For example, they may be able to go to a day centre or have a short stay in a hospice or residential home.
The person’s GP, district nurse or palliative care nurse should be able to help you access short-term care.
Residential and nursing homes offer short-term or long-term accommodation and care.
Your local authority Social Services can provide information about care homes, including what type of care they offer and any help you may be able to get with fees.
You can also talk to the person’s health professionals or social worker for more advice and information.
If the person you are caring for is admitted to hospital for cancer treatment, it is important that their care team knows that they have dementia and understands how it affects their needs.
If the person has a care plan, Advance Statement or ADRT, or if you have lasting power of attorney, ensure that their health professionals have a copy and are told if anything has changed.
If the person you care for becomes more unwell, they may be admitted to a hospice or a palliative care unit of the local hospital.
This may be short-term, for example to receive specialist treatment to control their symptoms, after which they return home.
Or they may be admitted at the end of life and stay there until they die, with treatment and support to keep them comfortable.
Hospices are generally smaller and quieter than hospitals and work at a gentler pace. Many encourage family and friends to visit and even stay overnight.
Hospice nurses can also visit terminally ill people at home and provide treatment to enable them to remain at home.
The person’s GP, district nurse, palliative care nurse or social worker can give you more information about hospices or hospital palliative care units.
To speak to a dementia specialist Admiral Nurse about depression, anxiety or any other aspect of dementia, call our free Dementia Helpline on 0800 888 6678 (Monday-Friday 9am-9pm, Saturday and Sunday 9am-5pm, every day except 25th December), email helpline@dementiauk.org or you can pre-book a phone or video appointment with an Admiral Nurse.
Our virtual clinics give you the chance to discuss any questions or concerns with a dementia specialist Admiral Nurse by phone or video call, at a time that suits you.
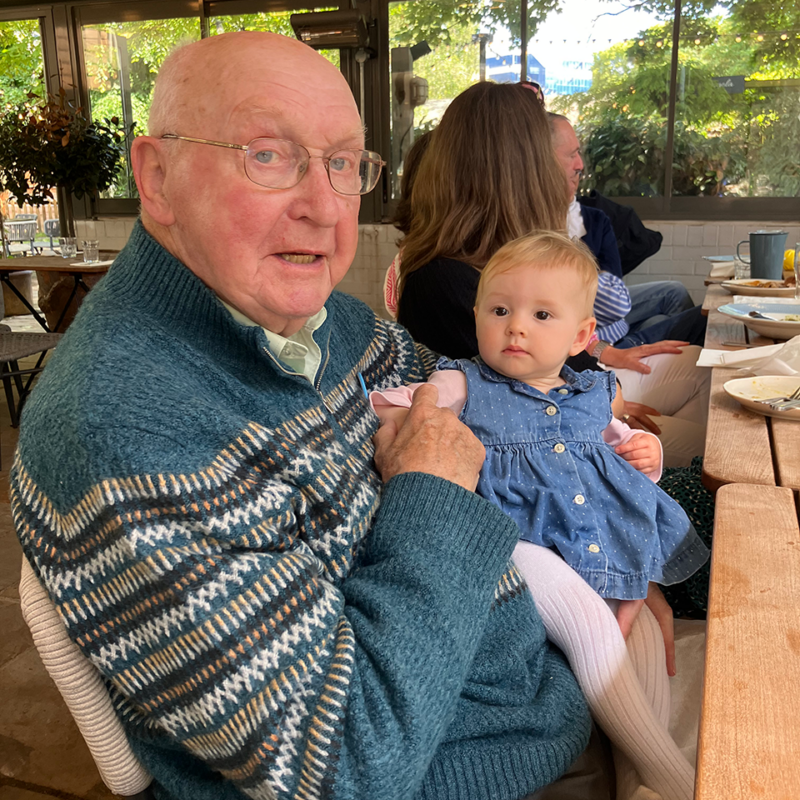
Simon, who has lived in New Zealand for two decades, discusses how he cares for his dad who has Alzheimer’s disease and lives alone in the UK.

Janet shares her experience caring for husband Ben and how they maintained the joy of Christmas after his diagnosis.

Shara reflects on her journey caring for Anna, her mother, who was diagnosed with vascular dementia in 2016.