Julie’s story: "I was let down by a system that doesn’t adequately support families affected by Lewy body dementia."
Julie writes about how her Admiral Nurse Rachel helped her understand the complexities of the health and social system – and her husband’s diagnosis – when no one else could.
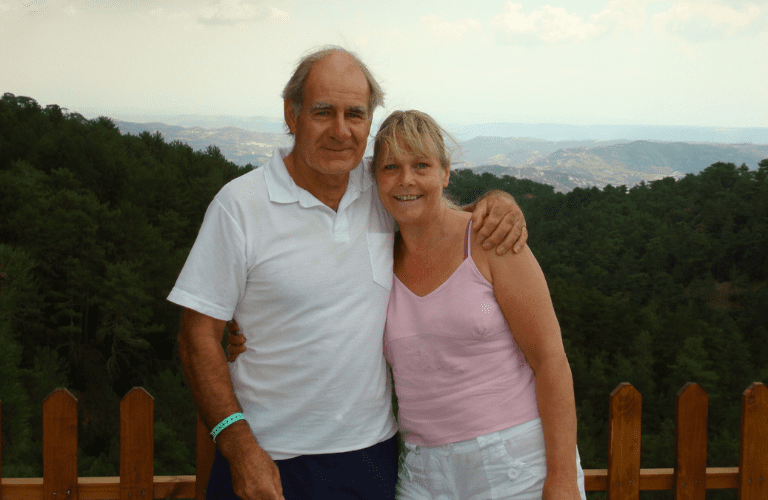
Julie and Brian on holiday in Cyprus
The first signs that things were not right were back in 2011 – Brian was 64. He used to be a plumber and was very good at DIY. He ended up making things worse instead of better and became quite forgetful – we just put it down to age.
In 2011 during a shopping trip, we were discussing what we were going to do with my mum and step-dad who were due to visit. Brian became angry and I had no idea why. He reached for the handbrake whilst the car was still in motion and I told him not to do that – I felt frightened, especially when there was a bus right behind us. He left the car when we had pulled over and we engaged in a cat and mouse chase, with Brian narrowly missing oncoming traffic.
I got him back into the car, but it was clear in my mind what I had to do. I phoned the doctor who said that he thought that there was something wrong for quite a while. I couldn’t understand why we hadn’t been told this sooner. Brian was then referred to the neurology department at Burton on Trent. We were given the initial diagnosis of Parkinson’s plus – whatever the plus means.
There weren’t any signs of tremors, which is what I associated with a diagnosis of Parkinson’s. If there were, they were very slight. The tremors started soon after. He was like a puppet on strings, with no body control.
After hospital transfer after hospital transfer, Brian eventually met a Consultant in Sheffield. He was prescribed medication which worked really well for the tremors. He got his mobility back, his tremors weren’t problematic, and things turned to a degree of normality for a short time.
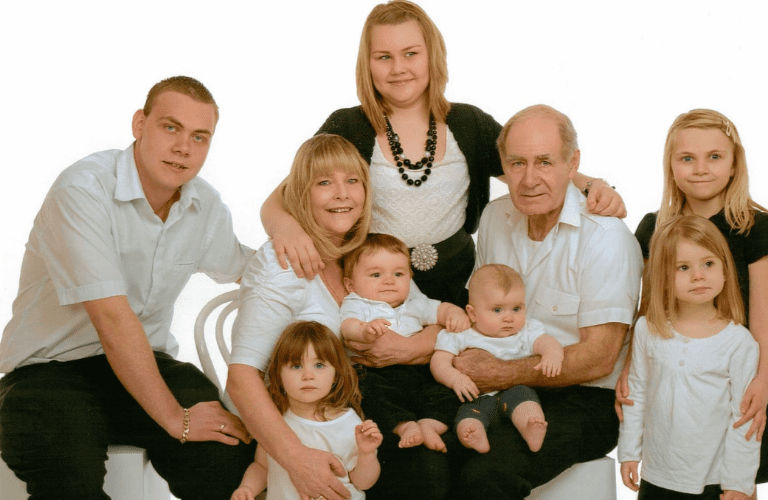
Julie and Brian with their grandchildren
Mounting worries
I became concerned when Brian would open the windows and shout at children who weren’t even in the street. He’d start to have delusions that I was having an affair with the neighbour’s grandson.
At points, he didn’t recognise me and would become confused and agitated. He felt like he was losing control. I didn’t know where to go for help. Do I phone the consultants? Was it normal? Was it not?
I wanted to call 111, I was anxious about Brian’s confusion, but he was adamant I was not to call them. I was becoming quite frightened of Brian and I didn’t know what his reaction would be if I made a phone call he didn’t want me to make.
A 24/7 carer
I was a 24/7 carer. It was sheer exhaustion. I’d be angry with Brian because I was so tired and then I’d feel guilty. Palpitations and dizziness became commonplace. In those short moments after I’d put Brian to bed and he was sleeping, I’d go into the garden and cry.
The delusions and hallucinations were becoming more intense. What was happening right now, I didn’t feel was Parkinson’s. I realised that I had to do something about this. I phoned the doctor and said I wanted a referral to a mental health team, or a dementia team. The doctor said that I should phone Dementia UK.
Meeting my Admiral Nurse
It was then that I met my Admiral Nurse, Rachel. I wouldn’t have been able to have carried on caring in our home without her. Rachel contacted the GP to request a referral to the adult mental health team. She also initiated the request for the referral for the Parkinson’s Nurse.
Rachel did a lot more than just the referrals. She gave me coping strategies for behaviour and stress. Rachel also helped me to understand the changes in Brian and why they were happening, including him just staring into space caused by cognitive and motor fluctuations. During these episodes Brian couldn’t talk, move or open his eyes. He could only respond with just a gentle squeeze of my hand. These episodes could last for up to nine hours.
No one else could tell me what was possibly causing this.
During one of these episodes, the Parkinson’s Nurse called for an ambulance. Before it arrived, Brian came round. Another episode occurred and I had to call the ambulance. He came round again when the paramedics arrived, but he was taken to hospital as a matter of caution.
A day later, I had a call from the hospital to say that he was end-of-life.
The hospital wasn’t the best place for him and he had tears in his eyes when I came to visit him, desperate for me to take him out. I’m thankful that I had the support of Rachel at this time. She sent me information about the PEG (tube feeding) as Brian couldn’t feed himself in the final few months. This helped me understand the implications of having this done, the risks for people with dementia, which includes infections, and helped in making a decision about what was best for Brian. Through Rachel’s input, I decided that caring for him at home was the best thing. And Rachel assisted with this by signposting me to palliative care teams.
A call for change
There isn’t enough knowledge out there around Parkinson’s and how dementia might relate. On some of the clinical letters, they mentioned Parkinson’s with dementia, and others just mentioned Parkinson’s. Others said that it was Parkinson’s cognitive problems. I still don’t have a clear answer to whatever it was that Brian was facing. And if I don’t know then how could health and social care staff provide him with the best care and support possible?
You don’t know where to go and what’s available to you. However I’m so thankful for the support of Rachel throughout; she helped me make sense of the fragmented health and social care system and provided understanding around Brian’s complexities when no one else could.
I’m sorry I did not do more to help you Brian, I just didn’t know what else I could do. I hope that this account helps others going through what we did – it’s only in hindsight that some of the pieces of the health and social care system jigsaw come together.
