Featured

Saïna’s story – A song for my beloved grandpa, Ralph
Saïna opens up about how her grandfather’s dementia has affected her, and how songwriting has provided a release.

Read personal stories from people living with a diagnosis, their family members and friends – as well as our dementia specialist Admiral Nurses.
Featured

Saïna opens up about how her grandfather’s dementia has affected her, and how songwriting has provided a release.
Featured
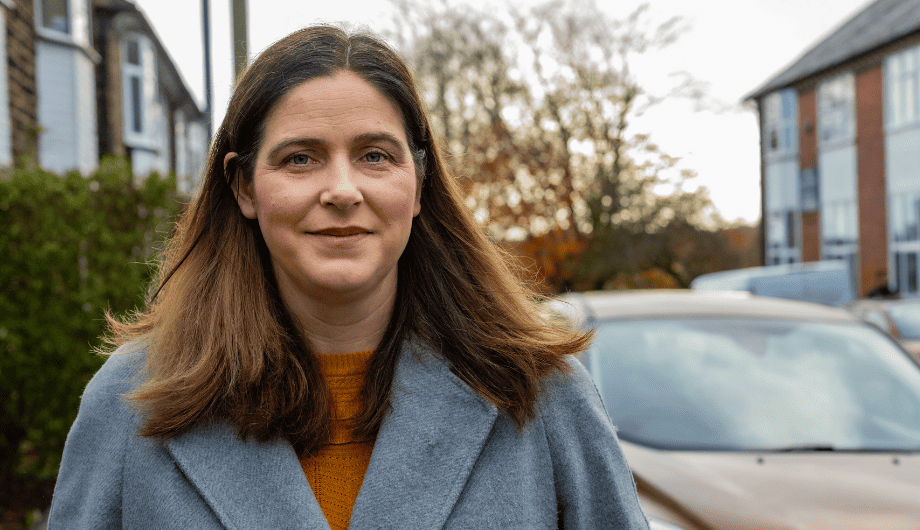
When her partner Andy was diagnosed with dementia at the age of 52, Christine struggled to know where to turn....

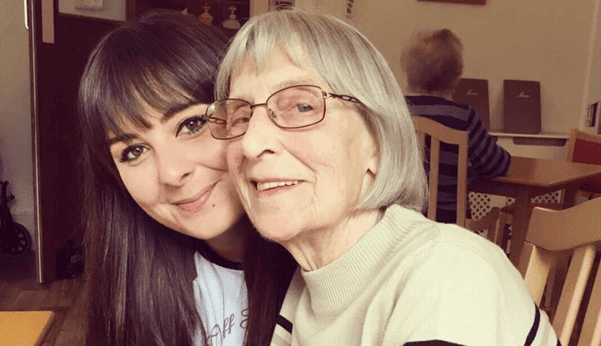
Ricky’s talks about how his Gran’s dementia diagnosis impacts his whole family and why he is supporting the ‘We live...

As a carer for her mum, who has vascular dementia, Clare is taking part in our ‘We live with dementia’...
Featured

Andy, 52, lives with young onset dementia. As part of our ‘We live with dementia’ campaign, he shares how his...
Featured

Peter shares why he and his puppy Murphy, will be taking part in Dementia UK's 10k Lapland Dash.
Featured

As part of Dementia UK’s ‘Fix the funding’ campaign, which is calling for an urgent review of the NHS continuing...
Jen, who works at tails.com, explains why she took on the October Dog Walking Challenge for Dementia UK.

When Steve’s mum, who had dementia, was hospitalised after a fall, Steve turned to Dementia UK’s Helpline for support.

Annette reflects on how the NHS continuing healthcare (CHC) funding application process is flawed for people living with dementia.
Featured
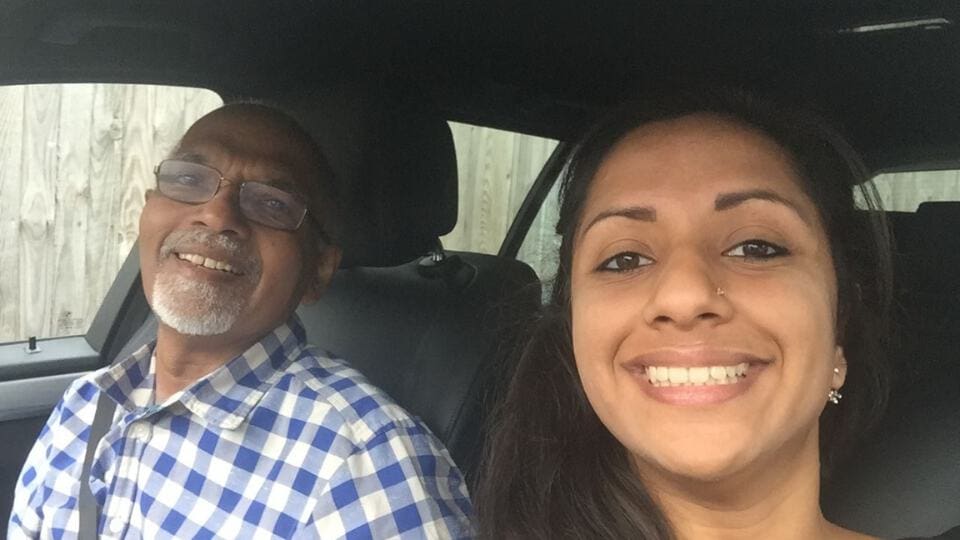
Eshaa shares how young onset dementia impacted her father's capabilities to communicate with his friends and family.

Adult Nursing lecturer and a PhD student Tidziwe reflects on the lack of awareness of dementia in her home country...

Heather shares her experience of attending a Closer to Home clinic with Admiral Nurse Debi.

Suzy reflects on the dementia journey of her mother, who was diagnosed with hydrocephalus in her 50s.